Claims can be rejected for a full invoice or an item within an invoice, and each is handled differently
Rejected claims for an item in an invoice
If an invoice item is rejected when performing a reconciliation, you will receive the message: 'Claim for service ID was rejected'.
To investigate why the item was rejected:
- From the Payments tab, double-click on the Payment ID.
- This will open the payment and the invoices it is for in the Claims tab.
- The invoice with the rejected item will have the Status COMPLETE as Medicare considers the claim complete.
- Expand the invoice.
- Review the items.
- The reason for the rejection will be displayed next to the Status.
- You can double-click an invoice or the patient to open the Patient Details screen, which provides easy access to Account Enquiry and Billing.
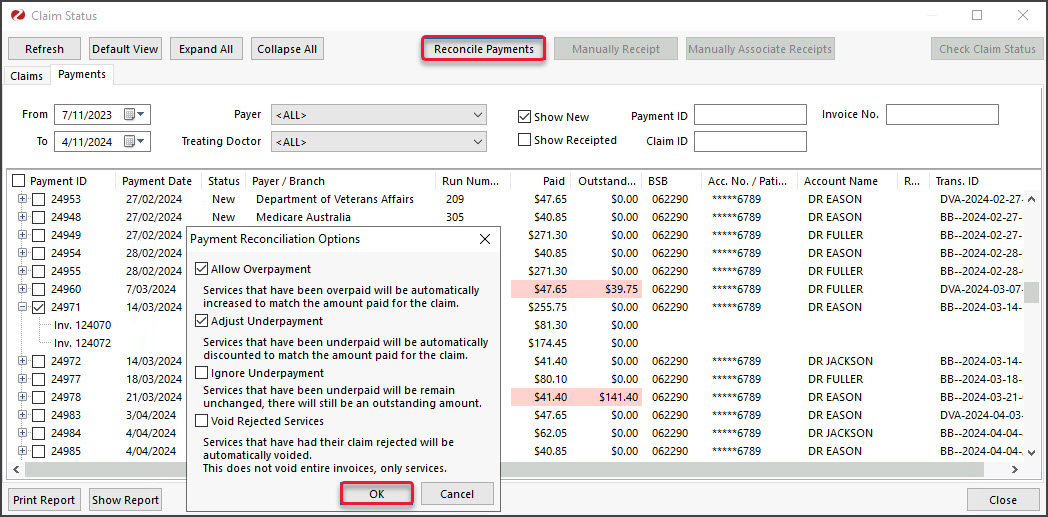
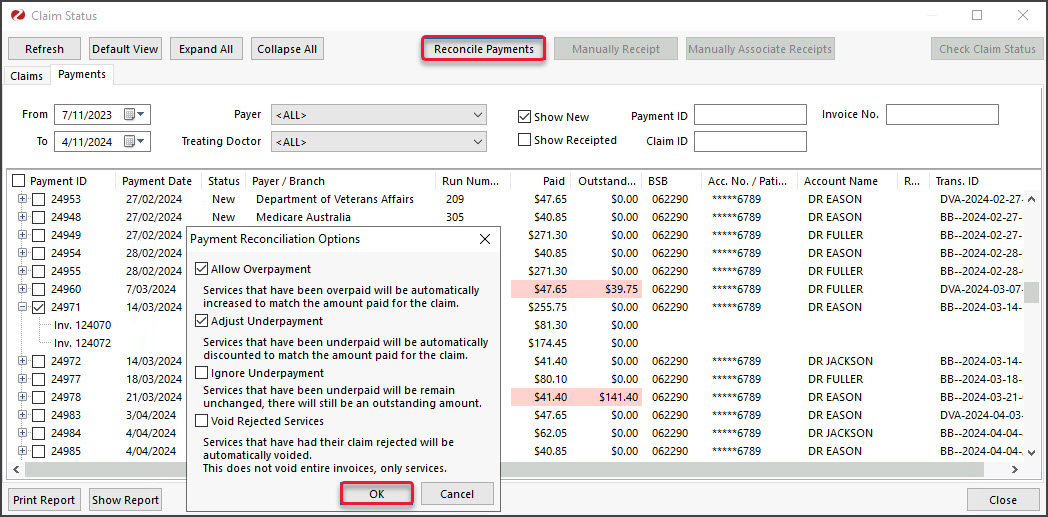
To void a rejected item:
- Go to the Payment tab and select the payment with the rejected invoice.
- Select Reconcile Payments.
- Tick the Void Rejected box on the Payment Reconcile Options dialog.
- Select OK.
Rejected claims for full invoices
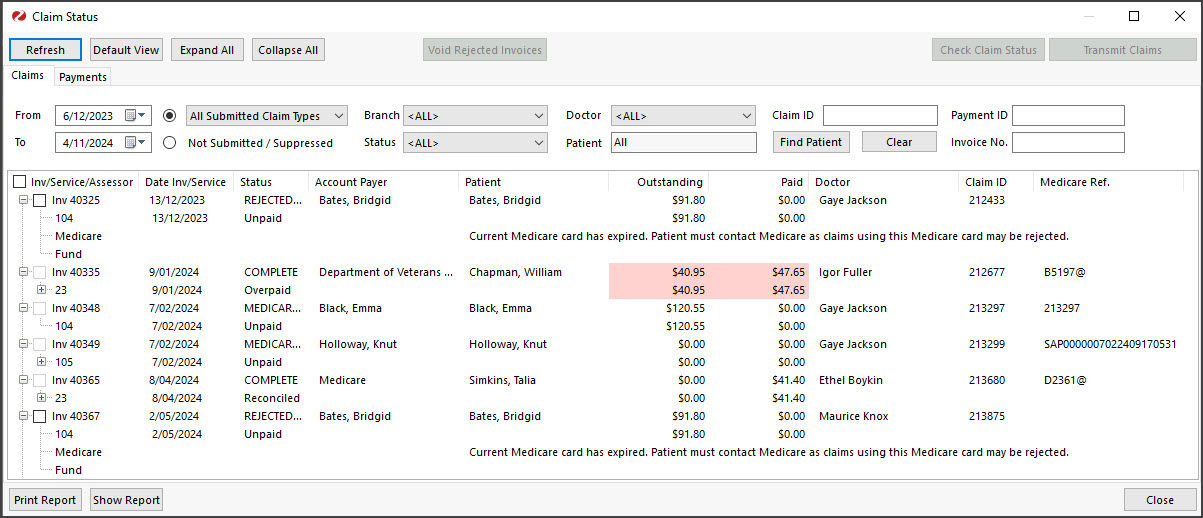
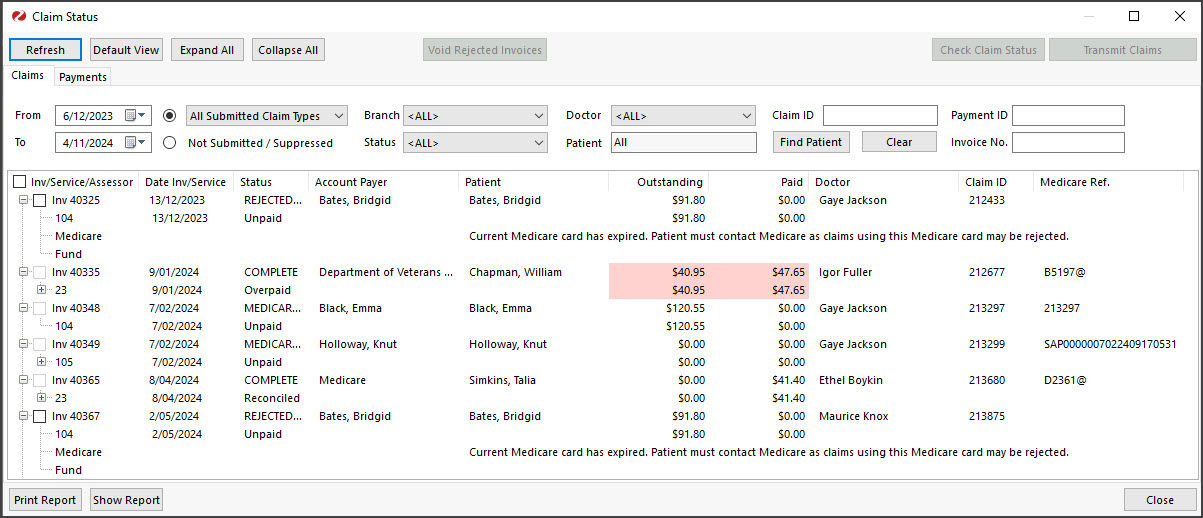
If a full invoice is rejected, it will not appear in the Payments tab, as there will be no payment. It will appear in the Claims tab, so you need to review the Claims tab regularly to review and void rejected invoices.
To process rejected claims for full invoices:
- Go to the Claims tab.
- Select Rejected from the Status field.
- Select Refresh.
All rejected invoices will appear. - Expand each invoice to see the reason for the rejection next to the Status.
- Take any required actions, such as reinvoicing the rejected invoice.
- Select the invoice/s to be voided.
- Select the Void Rejected Claims button.
- Confirm the action.
Repeat these steps for each Rejected Status under Status. For example, Rejected Fund.