Give selected staff access to the Claims Status screen so they can manage outgoing claims and incoming payments. This screen is accessed via the Management tab's Claims button, and access is granted by adding the Claiming function to the role used to restrict access to claims and payments.
Access control overview
Zedmed uses 'Functions' to give access to specific features and processes, and these functions are grouped into 'Roles'. Staff accounts are given one or more roles based on what they need to have access to in Zedmed. For example, if you get a new nurse, you just create an account and give it the Nurse role, which will contain all the functions a nurse needs.
By default, the Administrator role has the Claims function, so staff with the Administrator role do not need any access changes to be able to use the Claims Status screen.
To learn more, see the Review Claims and Reconcile Payments guides and the Accounts & Security guide.
Giving Access to the Claims Status screen
To give access:
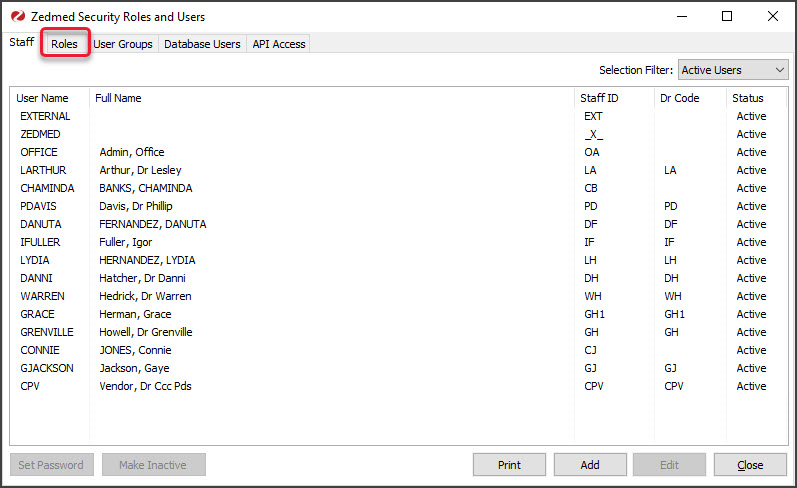
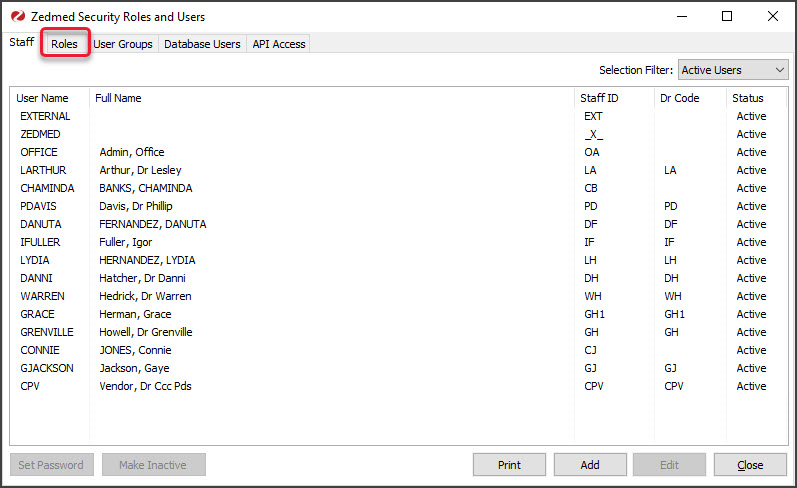
- Go to Zedmed's Utilities tab.
- Select Security.
The Zedmed Security Roles and Users screen will open. - Select the Roles tab.
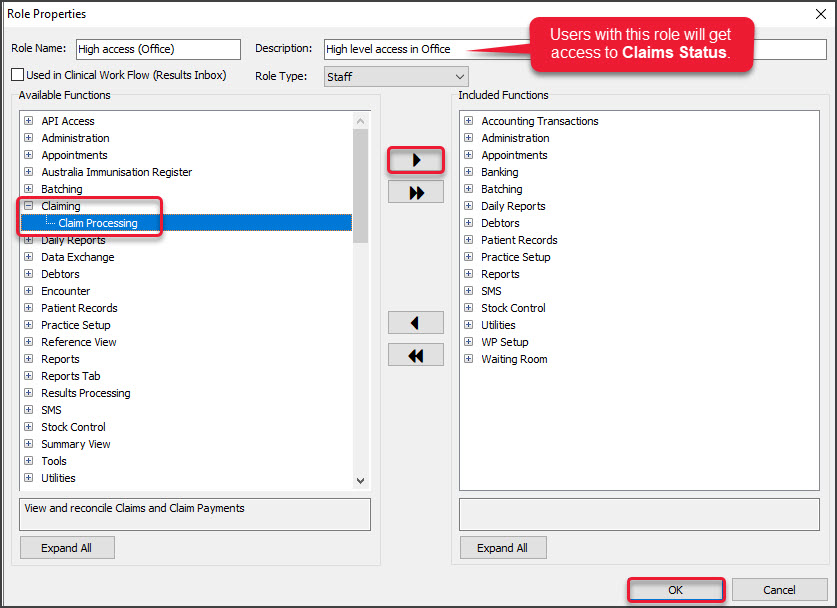
 The Role Properties screen will open.
The Role Properties screen will open. - Select the role that allows staff to manage outgoing claims and incoming payments.
This is the role that would have been given staff access to batching and ECLIPSE claims and payments before the Zedmed v35 upgrade.Note: If no role is currently used to manage access to claims/payments, select Add on the Security Roles and Users screen to create a new role, add the Claims Processing function to that role, and then use the Staff tab add the new role to all the staff who require claims/payments access. For more information, see the Accounts & Security guide. - In the left pane, expand the Claiming function and select Claim Processing.
- Select the Right-facing arrow.
- Claiming will be added to the Included functions on the right pane.
- Select OK.
All staff with the 'Role' you added the Claim Processing 'Function' to will now be able to use the Claims Status screen.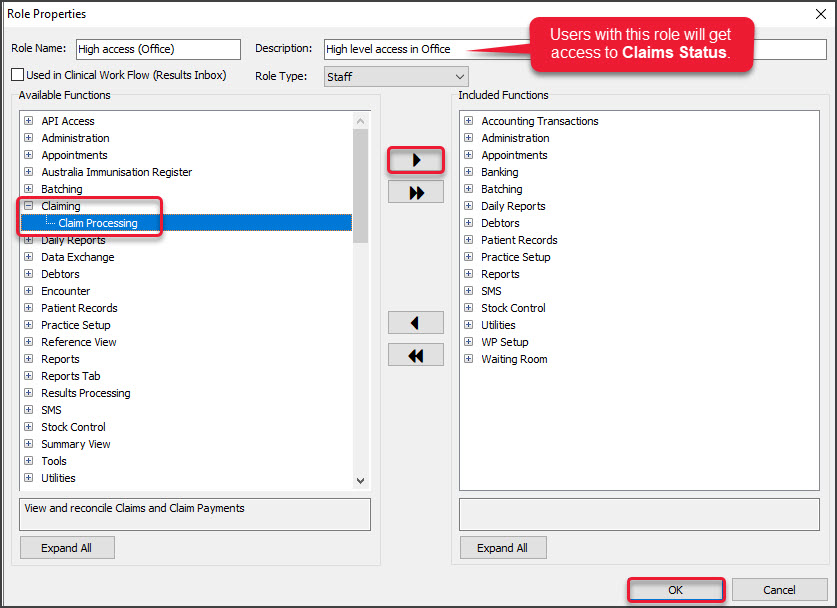

 The Role Properties screen will open.
The Role Properties screen will open.