For the Zedmed v35 migration, invoices were held back to ensure there were no Medicare, ECLIPSE or Tyro batches waiting to be transmitted or awaiting a response before the upgrade. After the upgrade, these invoices need to be submitted, and how to do this is explained in this guide.
The new claims process
Zedmed's implementation of Medicare’s web services model means invoices are no longer batched in Zedmed before being sent. Instead, when you create an invoice the claim is automatically transmitted. This process is managed in the new Claims Status screen, which has a Claims tab to show Submitted and Not Submitted invoices and a Payment tab where remittance advice and payments are received and reconciled.
This new streamlined process means Medicare, DVA and Health Fund claims all use the same automated process. To learn more, see the new Review Claims and Reconcile Payments articles.
Submitting Medicare & DVA bulk bill claims
The Zedmed v35 Claims Status screen has a Transmit Claims feature that submits groups of held invoices. After the upgrade, all held bulk bill and DVA invoices will appear in the Claims Status screen and can be submitted together using Transmit Claims.
Important: If you have voided any of the invoices you are going to submit, ensure that you have contacted Medicare and advised them not to pay the voided invoices. Zedmed will not be able to reconcile a payment if Medicare has paid for an invoice that is voided in Zedmed. This means all invoices covered by that payment will need to be manually receipted.
Pre-requisite: staff submitting invoices will need to be given Claims Processing access.
To submit held bulk bill invoices:
- Go to Zedmed's Management tab.
- Select Claims.
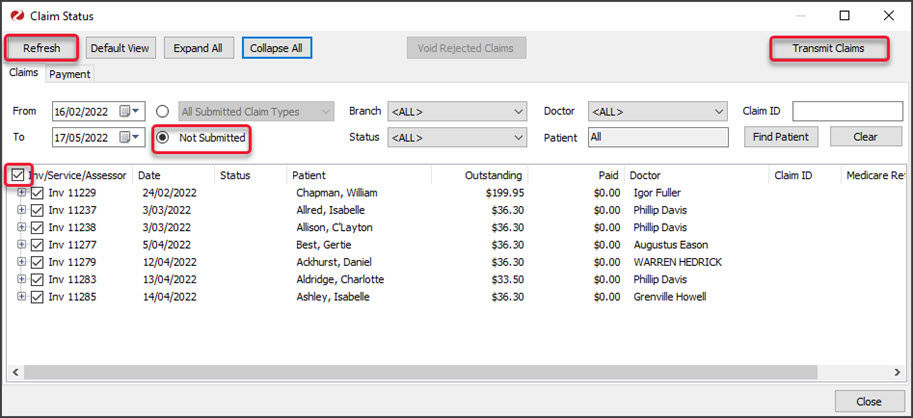
The Claims Status screen will open. - Select Not submitted.
All the held invoices will display.
You can filter the invoices shown by using the From and To fields to select the date range the invoices were held for - Select the Refresh button.
- Select the tick box beside Inv/Services/Assessor.
The invoices will be ticked. - Select Transmit Claims.
All the held bulk bill and DVA invoices will be sent to Medicare.
You can then process the payments as documented in the Reconcile Payments article.
If you encounter any errors, see the troubleshooting guide.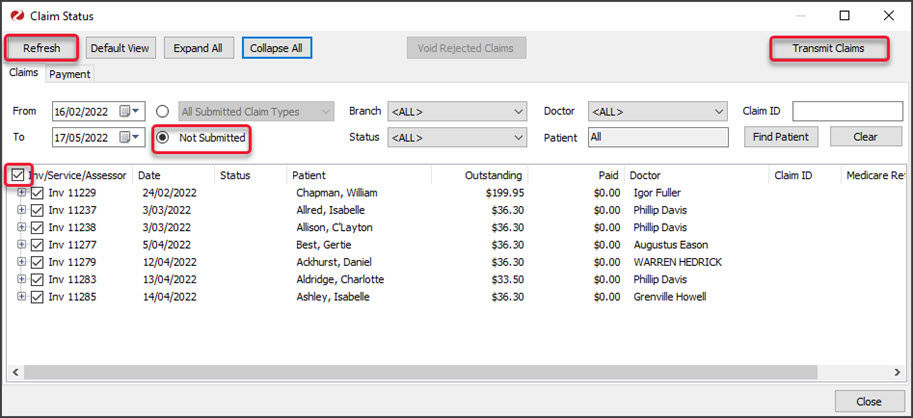 Watch these steps in our submitting invoices video
Watch these steps in our submitting invoices video
Submitting ECLIPSE claims
After the upgrade, held ECLIPSE invoices are sent by opening each invoice in the patient's record and selecting ECLIPSE. The invoices will be submitted and you can view them in the Claim Status screen's Claim tab while waiting for the remittance advice.
Pre-requisite: staff submitting invoices will need to be given Claims Processing access.
To submit an ECLIPSE Invoice:
- Go to Zedmed's Reception tab.
- Select Patients then locate the patient and open their record.
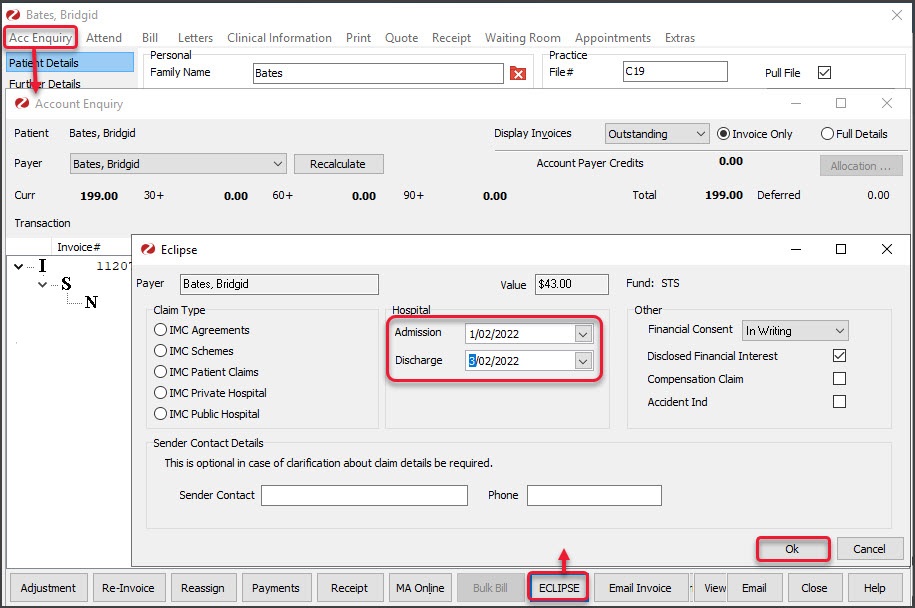
To learn more, see the open a patient's record article. - Select Acc Enquiry on the top menu.
The Account Enquiry screen will open. - Select the Invoice that has not been sent. The ECLIPSE button will be selectable for an unsent claim.
Make sure the patient is the payer, as this is a requirement for ECLIPSE payments. - Select the invoice.
- Select ECLIPSE.
The ECLIPSE screen will open. - Select the Admission and Discharge dates.
- Select the Financial Consent.
- Select OK.
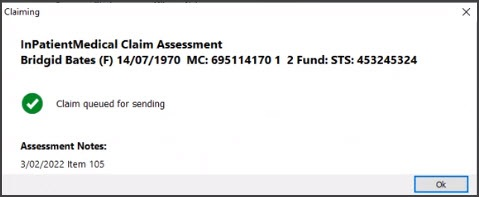
 The InPatient Medical Claim Assessment dialog will open and confirm if the claim was sent.
The InPatient Medical Claim Assessment dialog will open and confirm if the claim was sent.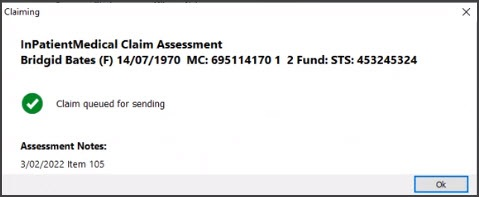
- Select OK.
The claim will be sent and no further action is needed. You can view the sent claim in the Claims Status screen.
If you encounter any errors, see the troubleshooting guide.
Watch these steps in our submitting invoices video

 Watch these steps in our submitting invoices video
Watch these steps in our submitting invoices video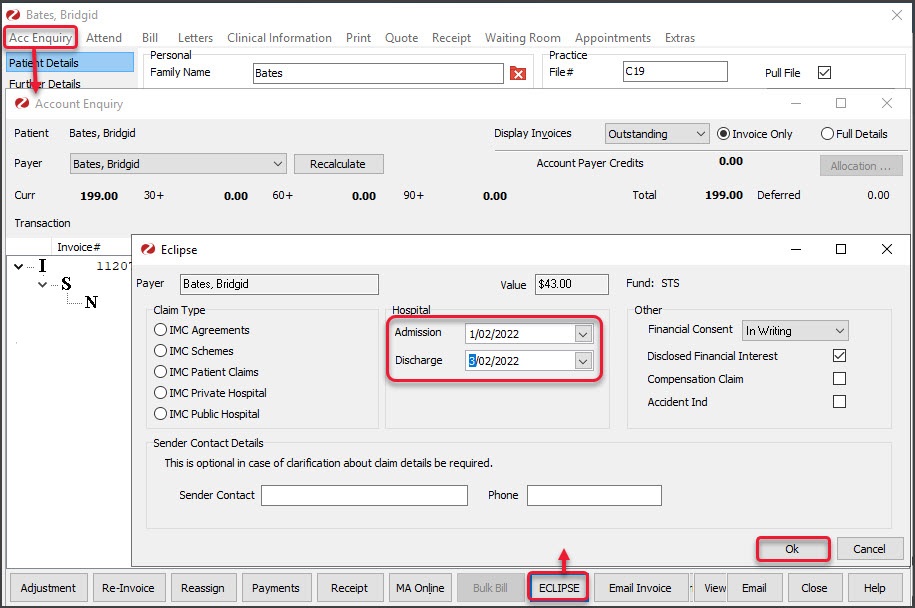 The InPatient Medical Claim Assessment dialog will open and confirm if the claim was sent.
The InPatient Medical Claim Assessment dialog will open and confirm if the claim was sent.